Currently Empty: $0.00
Scoliosis Surgery in Hyderabad: Advanced Care for a Better Life
Complete Guide to Scoliosis Surgery in Hyderabad: Types, Procedures, cost and Recovery Timeline.
Understanding Scoliosis and Surgery
Definition of Scoliosis
Scoliosis is a medical condition characterised by a lateral or sideways curvature of the spine. This curvature can present itself in the form of an “S” or a “C” shape, predominantly developing in children during their growth spurts before puberty. While some spinal curves remain mild and require minimal intervention, others can be severe, potentially leading to discomfort, chronic back pain, and even respiratory issues due to the distortion of the rib cage affecting lung function.
Indications for Surgery
Surgical intervention for scoliosis becomes necessary under specific conditions. Typically, surgery is considered when:
The spinal curvature exceeds 45 degrees and continues to progress.
The curvature causes significant pain that cannot be managed through conservative treatments.
There is a noticeable deformity affecting the patient’s posture and appearance, impacting their quality of life.
Non-surgical treatments such as bracing and physical therapy have failed to halt the progression of the curve.
The curvature leads to complications such as respiratory or cardiac issues due to the misalignment of the spine.
Types of Spinal Curves
The type of spinal curve has a substantial impact on treatment decisions in scoliosis. Understanding the nature of the curve is crucial for determining the appropriate intervention. The spinal curves are generally classified as follows:
Thoracic Curves: Curves in the upper back region are often more apparent and can cause asymmetry in the shoulders and rib cage. These curves are commonly addressed through bracing or surgery, depending on severity and progression.
Lumbar Curves: Curves in the lower back, which may lead to imbalance in the hips and lower spine. These require careful evaluation to determine whether surgical correction or non-invasive methods would be most beneficial.
Thoracolumbar Curves: These curves span both the thoracic and lumbar regions, necessitating a comprehensive treatment plan that may involve a combination of bracing and surgical intervention.
Double Major Curves: Characterised by two primary curves, often one in the upper spine and one in the lower spine. Treatment strategies for double major curves are typically more complex and may include multiple surgical techniques to achieve the best possible outcome.
An understanding of the specific curve type helps medical professionals to tailor the treatment plan to the individual’s specific condition, thus maximising the effectiveness of both surgical and non-surgical treatments.
With a thorough understanding of scoliosis and the indications for when surgery becomes necessary, patients and healthcare providers can make informed decisions about the optimal course of treatment, ensuring the best possible outcomes.
Types of Scoliosis Surgery Procedures
Spinal Fusion Surgery
Spinal fusion surgery is widely recognised as the primary surgical treatment for severe scoliosis. The goal of this surgery is to correct the spinal curvature by fusing two or more vertebrae so that they heal into a single, solid bone. This procedure stabilises the spine and prevents further curvature.
Use of Metal Rods and Implants
During spinal fusion surgery, metal rods and implants are often used to provide additional support and alignment to the spine. Surgeons attach these rods to the spine using screws and hooks. These metal instruments help maintain the spine’s corrected position as the bones fuse together. Over time, the bones grow around the rods, making them a permanent part of the spine. This method ensures both structural support and long-term stability.
Minimally Invasive Surgical Options
Minimally invasive surgical options are becoming increasingly common for scoliosis treatment, particularly in cases where the curvature is less severe. These procedures involve smaller incisions, leading to reduced pain and recovery time. Techniques such as thoracoscopic spinal surgery allow surgeons to correct spinal deformities through small incisions using specialised instruments and cameras. Although not suitable for all scoliosis cases, minimally invasive methods offer a viable option with fewer risks and quicker recovery times compared to traditional open surgery.
A thorough understanding of these surgical options is essential for making informed treatment decisions. Evaluating the severity of the curvature and discussing the potential benefits and risks with your healthcare provider is a crucial step in the surgical journey.
Pre-Surgery Diagnostic Requirements
Essential Imaging Tests
Before any surgical intervention for scoliosis, a series of imaging tests are mandatory to ascertain the severity and specifics of the spinal curvature. The essential imaging tests include:
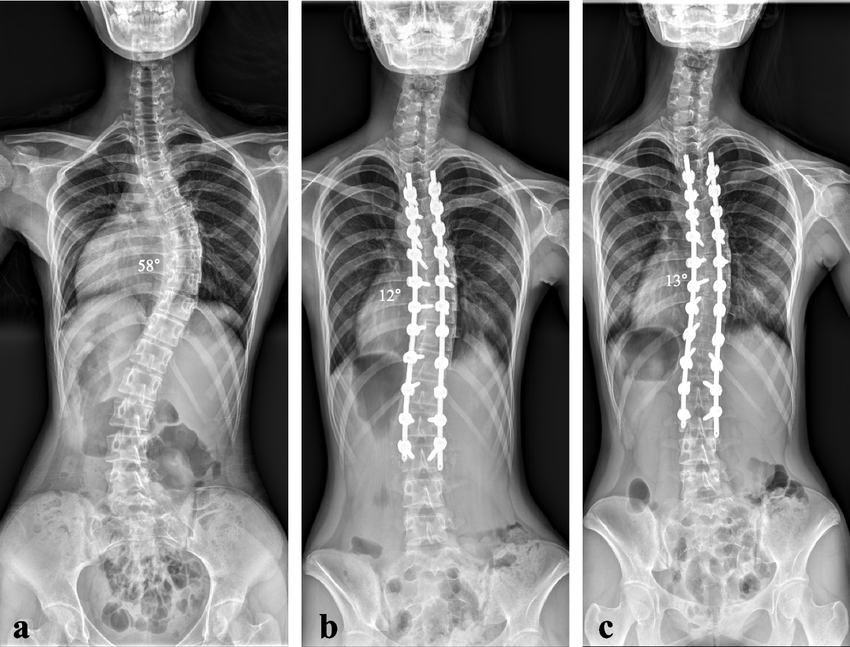
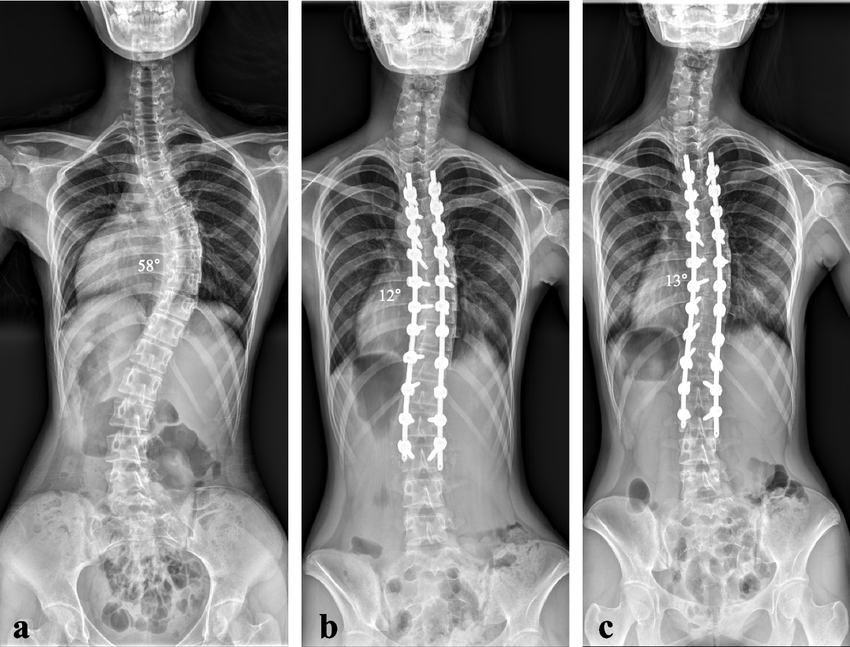
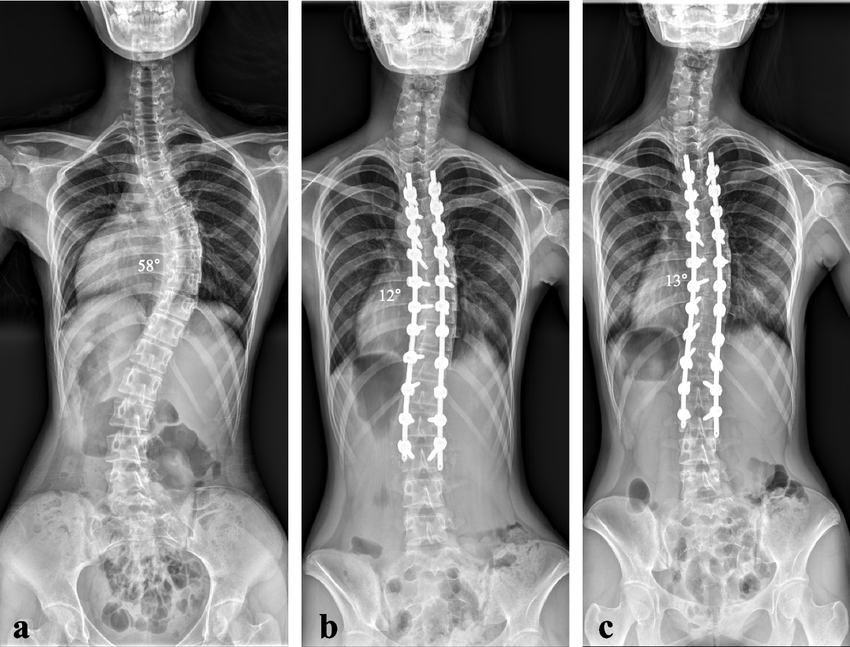
X-rays: These provide a primary view of the spine’s alignment and curvature. They are crucial for measuring the angle of the scoliosis curve.
CT Scans: Computed Tomography (CT) scans offer a more detailed cross-sectional view of the spine. These scans help in understanding the severity of the curvature and any associated structural anomalies.
MRI: Magnetic Resonance Imaging (MRI) is used to visualise the spinal cord, nerves, and soft tissues. It is particularly useful in identifying any compression or involvement of neurological structures.
These imaging techniques collectively allow for a comprehensive assessment, ensuring the surgical plan is tailored accurately to the patient’s needs.
Physical Examination and Medical History Evaluation
A thorough physical examination, accompanied by a detailed medical history evaluation, is pivotal in preparing for scoliosis surgery. During the physical examination, the surgeon assesses the patient’s spinal alignment, range of motion, and any observable symptoms such as uneven shoulders or hips. The medical history evaluation includes:
Previous medical conditions or surgeries
Family history of scoliosis or similar conditions
Symptoms such as pain, breathing difficulties, or physical deformities
The goal is to identify any factors that could influence the surgical outcome or necessitate additional preoperative interventions.
Assessment of Curve Progression and Severity
Evaluating the progression and severity of the scoliosis curve is a critical step to determine the necessity and urgency of surgery. The progression assessment involves monitoring changes in the curvature over time, which is typically achieved through serial X-rays. Factors considered include:
Cobb Angle: This is the standard measurement used to quantify the severity of the spinal curve. Curvatures exceeding 45 degrees generally warrant surgical intervention.
Curve Pattern and Location: Different curvature patterns (thoracic, lumbar, thoracolumbar, or double major) influence the type of surgical approach required.
Patient’s Age and Growth Potential: Younger patients with ongoing growth spurts are monitored more closely for curve progression.
A detailed and comprehensive assessment using these methods ensures that the surgical approach is optimised, enhancing the likelihood of a successful outcome.
Comprehensive pre-surgery diagnostics not only guides the surgical plan but also contributes significantly to predicting post-operative recovery and long-term results.
Preparing for Scoliosis Surgery
Required Medical Clearances and Pre-operative Testing
Before undergoing scoliosis surgery, comprehensive medical clearances and pre-operative testing are essential. These assessments ensure that the patient is in optimal health and can safely undergo the procedure. The pre-surgery workup typically includes:
Imaging Tests: Essential imaging includes X-rays to provide detailed information about the spinal curvature, CT scans for more intricate details, and MRI to evaluate spinal cord and nerve involvement.
Blood Tests: These are conducted to check overall health and identify any potential issues such as anemia or infection.
Cardiopulmonary Evaluation: An assessment of heart and lung function is crucial, especially in severe cases where spinal curvature might impact breathing.
Medical History and Physical Exam: A thorough medical history review and physical examination ensure that any comorbid conditions are identified and managed appropriately.
Lifestyle Modifications and Physical Preparation
Preparing physically for scoliosis surgery can significantly impact recovery outcomes. Patients are often advised to adopt certain lifestyle modifications in the weeks leading up to surgery:
Exercise and Physical Therapy: Engaging in a light exercise regimen and physical therapy can help strengthen the muscles supporting the spine, potentially aiding in a smoother recovery.
Diet and Nutrition: Maintaining a balanced diet rich in nutrients supports overall health and optimises healing post-surgery.
Smoking Cessation: If applicable, patients are strongly encouraged to quit smoking, as it can impede healing and increase the risk of complications.
Mental and Emotional Preparation for Surgery
Undergoing scoliosis surgery is not just a physical challenge but also a significant mental and emotional milestone. Preparing mentally and emotionally can improve resilience and recovery:
Counseling and Support: Psychological counselling can be beneficial in managing anxiety and setting realistic expectations for surgery and recovery.
Educational Resources: Understanding the surgical process, potential risks, and expected outcomes can demystify the procedure and alleviate fears.
Support Groups: Connecting with others who have undergone scoliosis surgery can provide emotional support and first-hand insights.
Effective preparation before scoliosis surgery sets the stage for a successful operation and recovery. It involves a combination of thorough medical evaluation, lifestyle adjustments, and mental fortitude.
Transition
With a comprehensive understanding of pre-operative preparations, the next focus is on the actual surgical process. Here, we will delve into the steps involved, the types of anaesthesia used, and pain management strategies during and after the procedure.
The Surgical Process
Overview of the Surgical Procedure
Scoliosis surgery primarily aims to correct the spinal curvature and stabilise the spine. The most common procedure is spinal fusion surgery. Here’s a step-by-step explanation:
Anaesthesia: The patient is administered general anaesthesia to ensure they are unconscious and do not feel any pain during the surgery.
Incision: A vertical incision is made along the back, directly over the curved part of the spine.
Exposure and Preparation: The muscles and tissues are moved aside to expose the spine. The surgeon carefully prepares the vertebrae for fusion.
Bone Grafting: Bone graft material, usually taken from the patient’s pelvis or a donor, is placed along the spine. This acts as the scaffolding for the new bone to grow and fuse the vertebrae.
Placement of Metal Implants: Metal rods, screws, and implants are strategically placed to correct the curve and hold the spine in the new position while fusion occurs.
Fusion: The prepared vertebrae are then fused together using the bone graft, creating a solid spinal segment.
Closing the Incision: The muscles and tissues are moved back into place, and the incision is closed with sutures.
Types of Anaesthesia and Pain Management
General Anaesthesia: Ensures the patient is completely unconscious and pain-free during the surgery.
Epidural Anaesthesia: Occasionally used postoperatively for managing pain, providing continuous pain relief directly to the affected area.
Intravenous Pain Medications: Pain relief is achieved through IV medications, which can be controlled by the patient through a PCA (Patient-Controlled Analgesia) pump.
Duration and Hospital Stay Requirements
The duration of scoliosis surgery typically ranges from 4 to 8 hours depending on the complexity of the curvature and the number of vertebrae being fused. Post-surgery, patients usually stay in the hospital for 5 to 7 days for initial recovery and monitoring. During this period, pain management and early physical therapy are crucial to begin the healing process.
Transition to the Next Topic
Understanding the surgical process, including the procedure steps, types of anesthesia, and initial recovery period, sets the foundation for delving into the detailed recovery and rehabilitation phase.
Recovery and Rehabilitation
Immediate Post-Operative Care and Pain Management
Post-scoliosis surgery recovery begins with a comprehensive plan for immediate post-operative care and pain management. Following the procedure, patients usually remain in the hospital for 3 to 5 days. During this period, pain management is a critical focus. Various methods are employed to ensure patient comfort, such as the use of intravenous catheters, pain relief pumps, and oral medications. These approaches help control pain levels and facilitate early mobility. Physicians and nurses continuously monitor the patient’s vital signs and pain levels, adjusting the pain management regimen as needed.
Physical Therapy and Rehabilitation Timeline
Physical therapy is integral to recovery following scoliosis surgery. The rehabilitation process typically spans 3 to 12 months, divided into multiple phases to gradually increase mobility and strength.
First 3 Months: Initial recovery focuses on basic movements and pain management. Patients engage in light exercises, often under the supervision of a physical therapist, to promote healing and prevent stiffness.
3 to 6 Months: This phase introduces more intensive physical therapy targeting the improvement of core strength and flexibility. Patients may begin activities such as gentle walking and light stretching exercises.
6 to 12 Months: By this stage, patients can increase their activity level further. Physical therapy sessions focus on rebuilding muscle strength and improving overall fitness. Towards the end of this phase, many patients can return to most of their pre-surgery activities, though with some restrictions.
Gradual Return to Normal Activities and Restrictions
A cautious approach is essential for returning to normal activities post-surgery. Gradual reintegration into daily routines helps prevent complications and ensures a steady recovery:
First 6 Weeks: Patients are advised to avoid strenuous activities, heavy lifting, and extensive bending or twisting. Walking and basic physical therapies are encouraged to maintain circulation and muscle tone.
3 to 6 Months: Light aerobic activities such as swimming or cycling can be introduced. Lifting limitations may be incrementally increased, but patients should still avoid high-impact sports or activities that strain the spine.
Beyond 6 Months: Most non-strenuous activities can be resumed, but patients should consult their physician before engaging in high-intensity sports or activities that place excessive stress on the spine.
Patients’ commitment to their rehabilitation plan is crucial for optimal recovery and achieving the best long-term outcomes.
Benefits and Expected Outcomes
Correction of Spinal Deformity and Improved Posture
One of the primary benefits of scoliosis surgery is the significant correction of spinal deformity. Surgical intervention, particularly spinal fusion, aims to stabilize and realign the curved spine, improving overall posture. This correction alleviates the asymmetric physical appearance caused by scoliosis, such as uneven shoulders, hips, and a prominent rib cage, enhancing the patient’s self-esteem and quality of life. Post-surgery improvements in the spine’s alignment contribute to a more balanced and symmetrical body silhouette.
Prevention of Curve Progression
Another critical outcome of scoliosis surgery is halting the progression of the spinal curvature. Unchecked, severe scoliosis can lead to further complications, including compromised lung and heart function due to the distorted rib cage. Surgical intervention successfully stabilises the spine, preventing further curvature that could exacerbate these medical issues. By arresting curve progression, patients experience less pain and reduced risk of associated health problems.
Long-Term Success Rates for Different Age Groups
The long-term success rates of scoliosis surgery vary, but the outlook is generally positive across different age groups. In children and adolescents, where scoliosis is often detected early, surgical correction typically yields excellent results. Early intervention allows for more effective correction, given the spine’s greater flexibility during growth periods. Adults undergoing surgery can also expect substantial benefits; while their spines are less flexible, surgical outcomes still show significant improvements in both spinal alignment and overall function. Long-term studies indicate sustained correction and stabilisation of the spine, with many patients reporting reduced pain and enhanced physical activity levels post-recovery.
These benefits collectively underscore the importance of timely surgical intervention for scoliosis, offering patients a pathway to improved posture, halted progression of curvature, and long-term spine health.
Following these benefits, it is essential to be aware of the potential risks and complications associated with scoliosis surgery, which will be discussed in the next chapter.
Risks and Complications
Potential Surgical Complications
Scoliosis surgery, most commonly spinal fusion, comes with several inherent risks. Among the most significant are infection and nerve damage. Post-surgical infections, which can occur at the incision site or deeper within the spinal area, typically emerge a few days to weeks after surgery. Symptoms include redness, swelling, fever, and increased pain. Treatment usually involves antibiotics, and in severe cases, further surgical intervention may be necessary.
Nerve damage is another critical complication. The spinal cord and its associated nerves are highly susceptible during the operation. Damage can result in varying degrees of sensory or motor loss, potentially leading to partial or complete paralysis. Surgeons employ neuromonitoring techniques during surgery to mitigate this risk, yet it is not entirely avoidable.
Other notable complications include anesthesia reactions, blood loss requiring transfusions, and issues related to wound healing. Each of these risks necessitates thorough discussion and preparation with your surgical team ahead of the procedure.
Long-Term Implications and Hardware Issues
Following surgery, patients may face long-term implications, including potential hardware issues. Metal rods, screws, and other implants used to correct spinal curvature can sometimes fail, loosen, or irritate the surrounding tissues. Implant failure might necessitate additional surgeries for correction or removal.
Bone grafts, which are integral to the fusion process, also carry long-term risks. Incomplete fusion, known as pseudoarthrosis, can occur, leading to persistent pain and instability. Monitoring through regular follow-ups is critical to ensuring the bone fusion process completes as intended.
Impact on Mobility and Lifestyle
Post-surgery, mobility and lifestyle adjustments are often required. While the primary aim of the surgery is to halt curve progression and improve quality of life, the resultant stiffness from the fused section of the spine can limit flexibility. Activities requiring a full range of spinal motion may be restricted or modified.
Patients often experience prolonged rehabilitation periods, typically ranging from 3 to 12 months. During this time, physical therapy is crucial for regaining strength and adapting to any changes in mobility. Some lifestyle changes, such as avoiding heavy lifting and high-impact sports, become permanent considerations to avoid compromising the surgical outcome.
Understanding these risks and complications is essential for anyone considering scoliosis surgery. This comprehensive awareness allows patients and families to make informed decisions and prepares them for the potential challenges in the recovery journey.
Cost Considerations in Hyderabad
Scoliosis is a condition characterised by a sideways curvature of the spine. For severe cases, surgical intervention may become necessary. This chapter examines the financial aspects of scoliosis surgery in Hyderabad.
Average Cost Range
The cost of scoliosis surgery in Hyderabad generally ranges from ₹120,000 to ₹150,000. However, this is an average estimate and the actual expenses can vary significantly. Factors such as the hospital of choice, the surgeon’s expertise, and the specific nature of the surgical procedure will influence the total cost.
Factors Affecting Total Cost
Hospital Choice
Hospitals in Hyderabad differ in terms of facilities, quality of care, and overall reputation. High-end hospitals and specialised spine surgery centres often charge more for their services but may offer superior care and advanced technologies. The selection of a hospital may impact pre-operative, surgical, and post-operative costs, thereby influencing the total expenditure.
Surgeon Expertise
The expertise and experience of the spine surgeon play a crucial role in determining the cost. Surgeons who have extensive experience and specialised skills in scoliosis surgery typically charge higher fees. Nevertheless, their higher success rates and lower incidence of complications make them a preferable choice for many patients.
Specific Procedural Needs
The type of surgery and the techniques employed also affect the cost. For instance:
Spinal fusion surgery
Use of advanced metal rods and implants
Minimally invasive surgical techniques
These procedures may have varying costs based on the specific needs of the patient and the complexity of the condition. Additional costs can arise if complications occur or if additional treatments and extended hospital stays are necessary.
Insurance Coverage and Payment Options
Many hospitals in Hyderabad accept insurance, which can significantly reduce the financial burden of scoliosis surgery. Coverage varies based on the insurance provider and the specific policy. It’s essential to check:
If the hospital is in-network
The extent of coverage for pre-operative tests, the surgical procedure itself, and post-operative care
Out-of-pocket expenses and any exclusions
For those without insurance, several payment plans and financing options are available. Hospitals may offer instalment plans or work with medical financing companies to provide loans for surgery.
Understanding these cost considerations allows patients and their families to make informed decisions about scoliosis surgery, ensuring both the medical and financial aspects are carefully managed.
Post-Surgery Life and Support
Long-term Lifestyle Adjustments and Activity Modifications
Post-scoliosis surgery life involves numerous adjustments to optimise long-term outcomes and enhance quality of life. It’s imperative to integrate new lifestyle habits and modify existing routines to ensure a successful recovery and maintain spinal health.
Engaging in regular physical activity becomes crucial. Exercise regimes should be personalised and gradually intensified under the supervision of healthcare professionals. Low-impact activities, such as walking and swimming, are generally encouraged, while high-impact sports like running or contact sports should be avoided to prevent undue stress on the spine. Consistent physical therapy sessions help in strengthening the muscles supporting the spine, thereby improving overall postural stability.
Maintaining a balanced diet contributes significantly to the healing process. Nutrient-rich foods with ample protein, calcium, and vitamins facilitate tissue repair and bone health. Avoiding smoking and limiting alcohol consumption are also advised, as these habits can impede recovery and bone fusion.
Follow-up Care Schedule and Monitoring
Adequate post-operative care and regular monitoring are pillars of a successful recovery. Follow-up appointments typically commence within 2-4 weeks of the surgery, followed by periodic evaluations over the subsequent months and years, depending on the patient’s progress and specific needs.
During these appointments, healthcare providers will conduct physical examinations, review spinal alignment through X-rays, and monitor the integration of any implants used. Continuous assessment of curve progression or any potential complications is crucial to adjusting the treatment plan as required.
Typically, the follow-up care schedule includes:
Initial Post-Surgery Appointment: 2-4 weeks after surgery.
Bi-Monthly Check-ups: For the first six months.
Quarterly Evaluations: In the first year post-surgery.
Annual Check-ups: Thereafter, to monitor long-term outcomes.
Support Groups and Resources for Patients
Support systems play a vital role in helping patients and their families navigate the journey post-surgery. Connecting with others who share similar experiences offers emotional comfort, practical advice, and encouragement through recovery.
Joining scoliosis support groups provides a platform to exchange stories, discuss challenges, and celebrate milestones. Online forums and local community groups can be valuable networking resources.
Additionally, engaging with healthcare practitioners, such as physical therapists, orthopaedic specialists, and mental health counsellors, ensures a holistic approach to recovery, addressing both physical and emotional needs.
Overall, embracing lifestyle adjustments, adhering to a structured follow-up care regime, and leveraging support networks significantly enhance post-surgery outcomes and contribute to a patient’s overall wellbeing.
The focus on these key aspects fosters a smooth transition to daily activities and a return to normalcy, setting the groundwork for long-term spinal health.
Frequently Asked Questions (FAQs) about Scoliosis Surgery
1. What level of scoliosis requires surgery?
Surgery is usually recommended when the spinal curve is greater than 40 degrees and shows signs of progression.
2. When do doctors recommend surgery for children with scoliosis?
Doctors recommend surgery for children with very severe curves of 45 to 50 degrees or higher.
3. What are the indications for scoliosis surgery in adults?
In adults, surgery may be considered if the spine’s curvature is severe or worsening significantly, accompanied by severe back pain unresponsive to other treatments.
4. What are the potential risks associated with scoliosis surgery?
Risks include implant failure, infection, bleeding, nerve injury, and blood clots, among other complications.
5. How long does recovery from scoliosis surgery typically take?
Full recovery from scoliosis surgery may take 6 to 12 months.
6. What are the common long-term side effects after scoliosis surgery?
Potential long-term side effects can include nerve damage, back pain, loss of flexibility, hardware malfunction, and muscle strain around the spine.
7. How soon can patients walk after scoliosis surgery?
Most patients can start walking the same day or the next day following scoliosis surgery.
8. What activities should be avoided after scoliosis surgery?
Patients should avoid heavy lifting, bending forward excessively, running, jumping, and driving until cleared by a doctor, typically 6–8 weeks post-surgery.
9. What is vertebral body tethering (VBT)?
VBT is a surgical procedure to correct scoliosis using a flexible tether attached to the spine, allowing for growth and maintaining flexibility.
Take the first step toward hassle-free hernia treatment today! At Magicward, we make it simple to compare surgery costs and find the best hospital tailored to your needs. Fill out the form now to receive personalized quotations from top hospitals in Hyderabad. Your health is our priority—let Magicward guide you to the right care at the right price!
