Currently Empty: $0.00
Relief from Anal Fissure: Best Surgery Options in Hyderabad
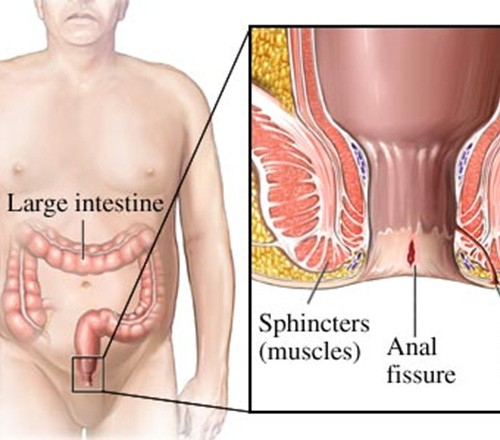
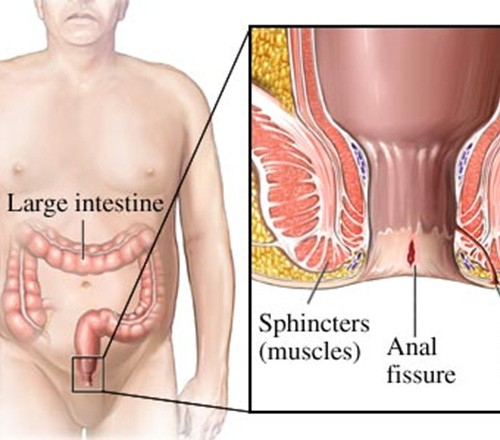
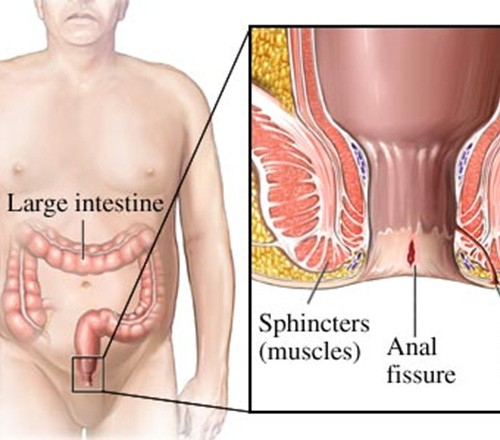
What is Anal Fissure Surgery?
Anal fissure surgery is a medical procedure aimed at treating tears in the lining of the anal canal, primarily when conservative treatments have failed to provide relief. This condition, marked by pain and bleeding during bowel movements, can become chronic if not adequately addressed, necessitating surgical intervention.
Purpose of Surgery
The primary goal of anal fissure surgery is to relieve symptoms and facilitate healing by reducing associated muscle spasms that hinder blood flow. This improves the chances for the fissure to heal efficiently while decreasing the occurrence of future fissures.
Anaesthesia
Anal fissure surgery typically requires general or regional anesthesia. This ensures the patient remains comfortable and still during the procedure, reducing the risk of complications.
Common Surgical Techniques
Lateral Internal Sphincterotomy
The most frequently performed technique for treating anal fissures is lateral internal sphincterotomy. This method involves making a small incision in the internal anal sphincter muscle, which helps to reduce spasm and pressure, promoting healing and providing significant pain relief. This procedure has a high success rate, making it a preferred choice among surgeons.
Fissurectomy
Another surgical option is fissurectomy, which involves the removal of the fissure and surrounding tissue. This approach often includes excision of any sentinel piles (small skin tags) that may have formed. The fissurectomy can be more extensive than sphincterotomy, and the wound is usually left open to heal naturally over time.
By understanding these surgical procedures and their purposes, patients can better appreciate the steps taken to alleviate their condition and promote recovery.
With surgery clarified, the next critical phase involves determining the necessity for such an intervention, which we will explore in detail.
When is Anal Fissure Surgery Necessary?
Surgery for anal fissures becomes indispensable when non-surgical treatments fail to yield positive results. This necessity arises typically after one to three months of ineffectual medical therapy. Patients enduring persistent pain and bleeding despite adhering to conservative treatments find surgery to be a viable option to alleviate their symptoms and promote healing.
Failed Medical Therapy
Medical therapy serves as the frontline defence against anal fissures, employing various approaches such as topical nitroglycerin, calcium channel blockers, and botulinum toxin injections. Additional supportive measures, including warm sitz baths, dietary changes, and stool softeners, further aim to alleviate symptoms. However, when such measures prove inadequate over a period of one to three months, surgical intervention becomes the next logical step.
Persistent Pain and Bleeding
Chronic fissures are often accompanied by unrelenting pain and bleeding, which significantly affect the patient’s quality of life. These symptoms are not only distressing but also indicative of inadequate healing. The continuous discomfort, especially during bowel movements, necessitates a more definitive solution, making surgery an essential consideration in these cases.
Non-Responsive Chronic Fissures
Chronic fissures that resist topical medication and lifestyle modifications such as increased dietary fibre and improved toileting habits eventually require surgical attention. The internal anal sphincter spasms that contribute to chronic fissures impede blood supply to the fissure area, preventing proper healing. Surgical procedures like lateral internal sphincterotomy or fissurectomy specifically target these issues, offering a higher likelihood of relief and recovery.
Surgery, thus, becomes an imperative course of action under these circumscribed conditions. Understanding when surgery is necessary helps in timely intervention, ensuring that patients experiencing prolonged and severe symptoms receive the appropriate care. Subsequent sections will delve into the pre-surgery diagnosis and the types of surgical procedures available, providing a comprehensive view of the pathway from diagnosis to recovery.
Pre-Surgery Diagnosis
Physical Examination
The initial step in the pre-surgery diagnosis of an anal fissure involves a thorough physical examination by a healthcare provider. This examination aims to assess the fissure’s location and severity. Physicians typically ask about symptoms such as sharp pain during bowel movements, burning, itching, and visible bleeding. The patient is often positioned on their side or belly, and the doctor gently separates the buttocks to visually inspect the anal canal. If the pain makes it intolerable to continue, the healthcare provider may rely on observed symptoms for diagnosis rather than causing additional discomfort. In certain cases, a lubricated gloved finger may be gently inserted into the anus to gain a better understanding of the anal canal’s condition and to detect any muscle spasms contributing to the issue.
Medical History Review
A comprehensive review of the patient’s medical history is a crucial component of the pre-surgery diagnosis. This review helps to identify any underlying conditions or factors that might contribute to the development or persistence of anal fissures. Relevant aspects of the medical history include previous occurrences of anal fissures, instances of chronic constipation or diarrhoea, childbirth history (for female patients), and any other gastrointestinal disorders such as Crohn’s disease or irritable bowel syndrome. The healthcare provider also evaluates the patient’s lifestyle factors, such as dietary habits, fluid intake, and bowel movement patterns, to understand better the potential contributing causes of the fissure.
Additional Diagnostic Tests
To ensure a precise diagnosis and rule out other conditions, additional diagnostic tests may be necessary. These tests can include anoscopy or sigmoidoscopy, where a scope is gently inserted into the anus to provide a more detailed view of the anal canal and rectum. These tests help identify other potential issues such as haemorrhoids, abscesses, or fistulas which might mimic fissure-like symptoms. Moreover, if there are any signs of infection or inflammatory conditions, specific tests might be conducted to detect sexually transmitted infections (STIs) or inflammatory bowel diseases (IBD) like ulcerative colitis. A thorough diagnosis not only confirms the presence of an anal fissure but also helps in formulating an effective treatment plan and evaluating the necessity for surgical intervention.
Proper diagnosis is imperative in determining the appropriate course of action for treating anal fissures. With precise information on the fissure’s location, severity, and underlying causes, healthcare providers can tailor their treatment strategies to ensure effective and lasting relief for the patient.
Transitioning from diagnosis to preparation, it’s essential to understand the pre-operative steps required for a successful surgical outcome.
Types of Anal Fissure Surgical Procedures
Lateral Internal Sphincterotomy
Lateral Internal Sphincterotomy (LIS) is the most common and preferred surgical technique for treating chronic anal fissures. In this procedure, the surgeon makes a small incision in the internal anal sphincter to reduce muscle spasms. By reducing the muscle tone, blood flow to the area is improved, promoting healing of the fissure. This procedure is typically performed under general or regional anesthesia and is considered effective, with a success rate of approximately 95%.
The recovery period is generally short, with patients often able to return to normal activities within a week. However, potential complications include temporary incontinence, particularly to flatus and less commonly to faeces. Studies have shown incontinence rates of up to 36% immediately post-operation, though this is usually mild and transient.
Fissurectomy
Another surgical option is fissurectomy, which involves the removal of the fissure along with some surrounding tissue. This method aims to create a fresh wound that can heal more efficiently with better blood supply. Fissurectomy can be combined with other surgical procedures, like a sphincterotomy, to achieve better outcomes. Fissurectomy is considered when LIS alone might not be sufficient, or when the fissure appears complex.
Although effective, this procedure may result in a longer healing time compared to LIS and could potentially involve similar risks, including infection and bleeding. The decision to perform a fissurectomy typically depends on the specific characteristics of the fissure and the patient’s overall health condition.
Anal Dilation (Lord’s Operation)
Anal dilation, also known as Lord’s Operation, is a less commonly performed procedure due to its higher risk of complications. This technique involves manually stretching the anal sphincter to reduce spasms and improve blood flow. While it shares a similar goal with LIS, anal dilation has largely fallen out of favour due to a significant risk of causing permanent incontinence.
Research indicates that patient outcomes are less favourable with this approach, particularly concerning the long-term control of bowel movements. For this reason, anal dilation is usually reserved for specific cases where other treatments are not viable or have failed.
Choosing the appropriate surgical procedure requires a thorough evaluation by a colorectal specialist, considering factors like the patient’s health, the severity of the fissure, and previous treatments.
Proper diagnosis and treatment planning, as discussed earlier, are critical steps leading up to surgery. Post-surgery, patient recovery and aftercare are equally important to ensure successful healing and long-term relief from symptoms.
Preparing for Anal Fissure Surgery
Pre-operative Medical Evaluation and Clearance
Before undergoing anal fissure surgery, it is crucial to undergo a thorough pre-operative medical evaluation and obtain clearance from your healthcare provider. This evaluation ensures that you are in optimal health condition for the surgery and helps identify any factors that might complicate the procedure. The process typically includes a comprehensive review of your medical history, physical examination, and possibly some diagnostic tests such as blood work or an electrocardiogram (ECG) to assess your heart health.
Your healthcare provider will also inquire about any medications you are currently taking, including over-the-counter drugs, supplements, and prescription medications. Informing your doctor about any allergies, especially to anesthesia or medications, is also essential during this evaluation.
Discussion of Anesthesia Options and Risks
Anal fissure surgery is generally performed under general or regional anesthesia, and it is vital to discuss these options with your anesthesiologist. General anesthesia will render you unconscious during the surgery, while regional anesthesia will numb the lower half of your body but keep you conscious. Both types have associated risks and benefits, which should be thoroughly explained by your medical team.
Potential risks of general anesthesia include nausea, vomiting, sore throat, and, in rare cases, more severe complications like allergic reactions or breathing difficulties. Regional anesthesia poses risks such as headaches, back pain, or, in very rare instances, nerve damage. Understanding these risks and discussing any concerns with your healthcare provider will help you make an informed decision.
Following Specific Dietary and Medication Instructions Before Anal Fissure Surgery
Adhering to specific dietary and medication instructions before the surgery is critical for a successful procedure and smooth recovery. Your surgeon will provide clear guidelines on when to stop eating and drinking before the surgery. Typically, you will be advised not to consume any food or liquids for at least six to eight hours before the operation to reduce the risk of aspiration during anesthesia.
Additionally, you may be instructed to discontinue certain medications, such as blood thinners, non-steroidal anti-inflammatory drugs (NSAIDs), or any supplements that could increase bleeding risk. Your doctor might suggest alternatives or a schedule for safely pausing these medications. For those who suffer from chronic conditions such as hypertension or diabetes, your healthcare provider will guide you on managing these conditions leading up to the surgery.
Proper preparation for surgery is pivotal in reducing risks and enhancing recovery outcomes. By following the pre-operative medical evaluation, discussing anesthesia options thoroughly, and adhering to dietary and medication instructions, patients can approach the procedure with greater confidence and a clear understanding of what to expect.
As you prepare for the surgery, consider the post-operative care and lifestyle modifications necessary for a speedy recovery.
Benefits and Risks of Anal Fissure Surgery
Benefits
The primary benefit of undergoing anal fissure surgery is the long-term relief from pain and discomfort caused by chronic fissures. Many patients who have not found relief through conservative treatments such as diet modifications, topical ointments, or other non-surgical treatments find significant improvement post-surgery. Techniques such as lateral internal sphincterotomy (LIS) and fissurectomy commonly used in surgical interventions, not only aim to provide pain relief but also promote healing of the fissure. By reducing the pressure within the anal canal, these surgeries help improve blood flow to the affected area, facilitating a faster and more complete healing process.
Patients usually experience a marked reduction in symptoms like bleeding, itching, and discomfort during bowel movements. The overall improvement in the quality of life is a significant advantage, as patients can resume normal activities without the persistent discomfort that chronic fissures often bring.
Potential Risks
While the benefits of anal fissure surgery are profound, the potential risks and complications must also be considered. One of the most discussed risks is the temporary incontinence that affects up to 45% of patients immediately following surgery. This can range from mild difficulties in controlling gas to fecal incontinence. However, permanent incontinence is quite rare, and in most cases, any incontinence issues resolve within a few weeks to months post-surgery.
Rare complications can include infections at the surgical site, persistent bleeding, or an incomplete healing of the fissure. There is also a possibility of weakening of the anal sphincter muscle, which, while infrequent, can contribute to long-term incontinence issues. Scar tissue formation in the operated area might also occur, which can sometimes require additional interventions or prolonged healing time.
Furthermore, like any surgical procedure, there is a minor risk related to anesthesia, including adverse reactions, though such occurrences are uncommon and typically managed carefully by the medical team.
Considerations
Understanding these benefits and risks is crucial for patients and their healthcare providers when deciding on undergoing surgery for anal fissures. This balanced knowledge ensures that patients have realistic expectations and are well-prepared for both the recovery period and the potential outcome improvements.
After a successful surgery, maintaining a healthy lifestyle, including proper diet and hygiene, is essential to prevent recurrence and support optimal healing.
Recovery and Aftercare of Anal Fissure Surgery
Following anal fissure surgery, patients generally experience a manageable recovery phase. Most individuals can return home the same day as the surgery, provided they have someone to assist them initially. The body’s healing mechanism may take several weeks to achieve complete recovery, with a gradual reduction in symptoms over time.
Immediate Postoperative Phase
After the procedure, patients may feel discomfort or mild pain, which is typically managed with prescribed pain relief medications. It is important to maintain proper hygiene to prevent infections and promote healing.
Patients are advised to:
Take prescribed antibiotics as directed
Wash the surgical area gently with mild soap and water
Avoid using harsh, perfumed products on the affected area
Take Sitz baths for 10-15 minutes, two to three times a day, which involves soaking in warm water to support healing and provide relief from discomfort
Dietary Recommendations
Adopting specific dietary modifications can significantly aid in recovering from anal fissure surgery. Diet influences stool consistency and ease of bowel movements, which are critical in preventing strain during defecation.
Patients should:
Increase water intake to stay adequately hydrated
Consume a high-fibre diet, including fresh fruits, vegetables, and whole grains, to soften stools
Avoid spicy foods, caffeine, and alcohol as these can irritate the digestive tract
Consider taking stool softeners or fibre supplements as prescribed by their doctor
Gradual Healing
Recovery from anal fissure surgery is a progressive process. Patients can expect gradual improvement over several weeks. During this time, it is crucial to follow the postoperative care plan religiously. Engaging in light physical activities like walking can promote circulation and reduce the risk of complications.
Most patients achieve full recovery within a few weeks, regaining normal bowel function and significant pain relief. However, if symptoms persist or worsen, it is essential to contact healthcare providers for further evaluation.
Concluding Note
Effective postoperative care and adhering to recommended lifestyle changes are pivotal in ensuring successful recovery from anal fissure surgery. Maintaining a healthy diet, supporting proper hygiene, and following medical advice can facilitate the healing process and reduce the likelihood of recurrence.
For further guidance, patients should consult their healthcare provider, who can offer tailored advice based on individual health needs and circumstances.
Cost Considerations
Factors Influencing Anal Fissure Surgery Cost
The cost of anal fissure surgery in Hyderabad is determined by several factors. These include the hospital chosen, the length of the hospital stay, the specific surgical technique employed, and the type of facilities and equipment used. Typically, the price of the surgery ranges from ₹45,000 to ₹75,000.
Hospital Choice
Different hospitals may charge various rates depending on their infrastructure, reputation, and the expertise of their surgeons. High-end hospitals with advanced facilities might charge more compared to smaller clinics. The duration of the hospital stay, which can vary based on individual recovery needs, also impacts the total cost.
Surgical Techniques
The cost may vary based on the type of surgical technique used. Procedures like lateral internal sphincterotomy, which is the most common method, can have different price points compared to other techniques like fissurectomy or less common procedures like anal dilation. Surgical method impacts not only the initial cost but also the length of hospital stay and the recovery period, hence affecting the total expense.
Alternative Treatments
In addition to conventional surgery, alternative treatments like laser therapy are available. Laser treatments, although typically more expensive initially, may offer benefits such as no cuts or scratches, reduced bleeding, lesser pain, and quicker recovery times. These advantages might shorten hospital stays and reduce post-operative care costs, making them a viable option in the long term. The advanced laser treatment highlights these benefits.
Investing in the right treatment plan considering both immediate and long-term costs is essential for effective management and healing of anal fissures. The choice between conventional and laser treatment should be made after thorough discussions with your healthcare provider, considering all personal and financial factors.
Transitioning from the understanding of cost elements, one next considers practical aspects, such as the particular recovery measures and aftercare practices necessary to ensure successful healing and prevent recurrence of anal fissures.
Take the first step toward hassle-free hernia treatment today! At Magicward, we make it simple to compare surgery costs and find the best hospital tailored to your needs. Fill out the form now to receive personalized quotations from top hospitals in Hyderabad. Your health is our priority—let Magicward guide you to the right care at the right price!
